
Diagnosing a broken toe involves recognizing symptoms such as intense pain, swelling, bruising, and difficulty walking. Types of toe fractures include stress fractures, where small cracks form from repetitive stress, and traumatic fractures, resulting from a direct blow or impact. A doctor will perform a physical examination and may order X-rays to confirm the diagnosis and determine the fracture type. Relief options for a broken toe include rest and elevation to reduce swelling and pain. Depending on the type of fracture, buddy-taping the injured toe to an adjacent toe may provide support and alignment during healing. Wearing stiff-soled shoes can protect the toe and ease walking. In severe cases, a cast or surgery may be necessary to ensure proper healing. If you have fractured your toe, it is suggested that you consult a podiatrist who can guide you toward a comprehensive treatment plan.
Broken toes may cause a lot of pain and should be treated as soon as possible. If you have any concerns about your feet, contact Patrick Bruton, DPM from Big Country foot and Ankle. Our doctor will treat your foot and ankle needs.
What Is a Broken Toe?
A broken toe occurs when one or more of the toe bones of the foot are broken after an injury. Injuries such as stubbing your toe or dropping a heavy object on it may cause a toe fracture.
Symptoms of a Broken Toe
- Swelling
- Pain (with/without wearing shoes)
- Stiffness
- Nail Injury
Although the injured toe should be monitored daily, it is especially important to have a podiatrist look at your toe if you have severe symptoms. Some of these symptoms include worsening or new pain that is not relieved with medication, sores, redness, or open wounds near the toe.
If you have any questions, please feel free to contact our offices located in Abilene, and Brownwood, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
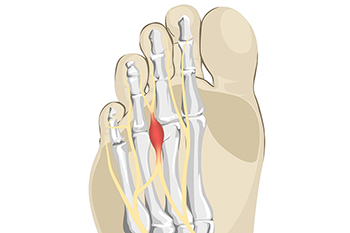
Morton's neuroma, named after the American surgeon Thomas G. Morton who first described it in the 19th century, is a painful condition affecting the nerves in the foot. This benign growth typically forms between the third and fourth toes, resulting from compression or irritation of the interdigital nerve. The exact cause of Morton's neuroma remains elusive, but factors such as wearing tight or high-heeled shoes, engaging in repetitive high-impact activities, or foot deformities may contribute to its development. Symptoms of Morton's neuroma often include a sharp, burning pain or sensation of a lump or foreign object in the ball of the foot. Individuals may also experience numbness, tingling, or a feeling of walking on a pebble. As the condition progresses, discomfort may worsen and become more persistent, particularly during weight-bearing activities. If you have pain in this part of your foot, it may be Morton's neuroma, and it is suggested that you visit a podiatrist. This type of doctor can accurately diagnose and effectively treat this condition.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Patrick Bruton, DPM of Big Country foot and Ankle. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our offices located in Abilene, and Brownwood, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.

Athlete's foot is a common fungal infection affecting the skin on the feet, particularly between the toes. Symptoms include itching, burning, and stinging sensations, often accompanied by redness, peeling, and cracking skin. The affected areas may also appear swollen and develop blisters. Diagnosis typically involves a physical examination by a podiatrist, who may scrape a small sample of the affected skin to examine under a microscope or send it to a lab for testing. Identifying the presence of fungal elements confirms the diagnosis. Early recognition and treatment of athlete's foot are essential to relieve discomfort and prevent the infection from spreading. Proper hygiene, antifungal medications, and keeping the feet dry and clean are effective measures to manage and prevent athlete's foot. Athlete’s foot can be uncomfortable and unsightly. If you have any of the above symptoms, it is suggested that you consult a podiatrist who can successfully treat this condition, which may include prescribed medication.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact Patrick Bruton, DPM from Big Country foot and Ankle. Our doctor will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our offices located in Abilene, and Brownwood, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.

